SAN DIEGO — People experiencing suicidal thoughts may not always be forthcoming in the deep pain they’re battling, but scientists are working to find ways to help them before they act. Researchers at the University of California San Diego School of Medicine have made a landmark discovery in the field of mental health, potentially leading to a blood test capable of detecting suicidal thoughts in individuals with major depressive disorder.
Depression is estimated to impact 16.1 million adults in the United States alone, incurring an annual cost of $210 billion. Traditionally, the condition has been associated with psychological symptoms. However, this new study highlights the significant physical dimensions of depression, specifically in cellular metabolism. Researchers are now focusing on markers of cellular metabolism as key indicators in studying mental illnesses, aiming to refine diagnostic and treatment approaches.
Key takeaways:
- Early warning: Identifying individuals at higher risk of suicide could be life-saving. Imagine a future where a simple blood test could flag those most vulnerable, allowing doctors to intervene early and prevent tragedies.
- Personalized treatment: The unique metabolic changes unveiled in the study offer potential targets for individualized treatment. Instead of a one-size-fits-all approach, doctors could tailor therapy based on a patient’s specific metabolic needs, perhaps including nutrient supplements like folate or carnitine to address identified deficiencies.
- New drug discovery: Understanding the role of mitochondrial dysfunction in depression opens doors for developing new drugs that target this critical cellular machinery. This could not only benefit those struggling with depression but also have broader implications for other chronic diseases linked to it.
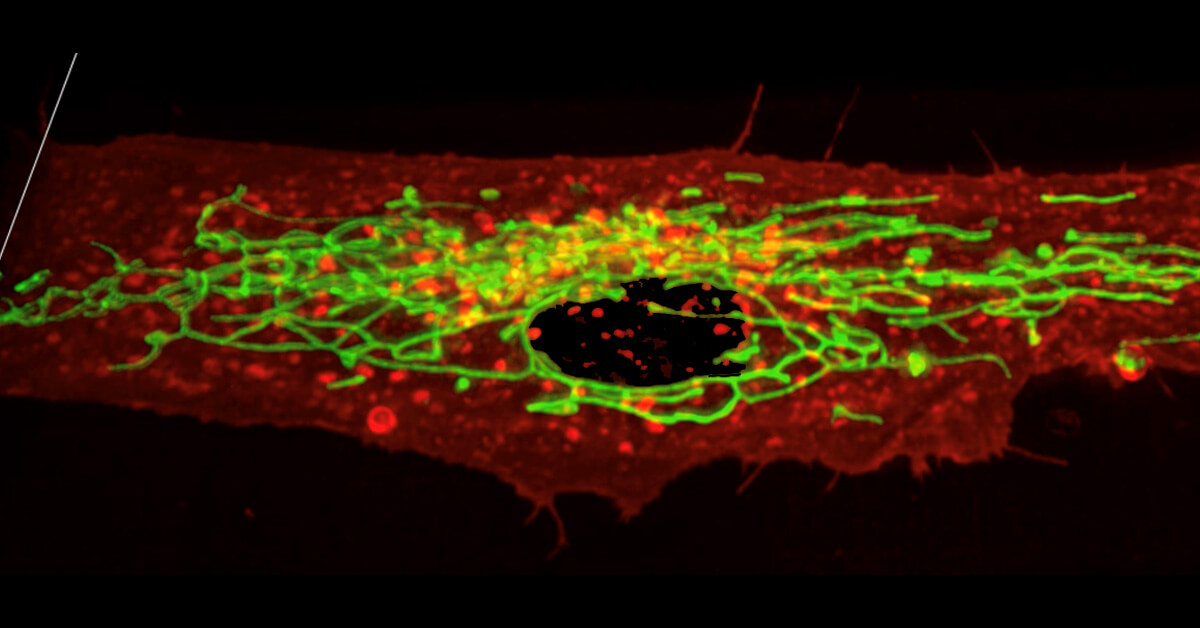
Imagine your cells as tiny factories buzzing with activity, fueled by microscopic power plants called mitochondria. When depression strikes, these factories and power plants can sputter and malfunction, throwing their delicate operations into disarray. Thanks to findings from this study, published in the journal Translational Psychiatry, there’s now the potential for development of a blood test that could detect suicidal thoughts in patients with depression.
To be sure, the research team analyzed blood samples from 99 individuals with treatment-refractory depression – a form of depression resistant to traditional therapies – who also experienced suicidal thoughts. They found unique patterns in five different chemicals circulating in the blood, acting like a subtle code revealing the metabolic changes associated with depression and suicidal ideation.
This remarkable ability to discern individuals at heightened risk for suicide based on blood metabolites could lead to a groundbreaking diagnostic tool.
“If we have 100 people who either don’t have depression or who have depression and suicidal ideation, we would be able to correctly identify 85-90 of those at greatest risk based on five metabolites in males and another 5 metabolites in females,” notes study co-author Robert Naviaux, MD, PhD, in a statement. “This could be important in terms of diagnostics, but it also opens up a broader conversation in the field about what’s actually leading to these metabolic changes.”
Metabolomics, the study of chemical processes involving metabolites, has played a pivotal role in this research. Naviaux highlights the importance of this technology in understanding how body chemistry influences mental states and behaviors. The identification of specific biomarkers related to suicidal ideation underscores the potential of metabolomics in transforming mental health diagnostics and treatment.
“Mental illnesses like depression have impacts and drivers well beyond the brain,” says Robert Naviaux, MD, PhD, a professor in the Department of Medicine, Pediatrics and Pathology at UC San Diego School of Medicine. “Prior to about ten years ago it was difficult to study how the chemistry of the whole body influences our behavior and state of mind, but modern technologies like metabolomics are helping us listen in on cells’ conversations in their native tongue, which is biochemistry.”
Of course, the possibility of a blood test for detecting suicidal thoughts opens new doors in personalizing mental health care. Such a test could allow for early intervention in high-risk individuals, potentially saving lives. Furthermore, this research paves the way for exploring novel treatment approaches, such as supplementing specific metabolic deficiencies.
Naviaux notes that while no single metabolite is a cure-all, supplementing metabolic deficiencies with compounds like folate and carnitine might nudge metabolism in a beneficial direction. This approach could enhance treatment responsiveness and, critically, prevent suicides.
“Many chronic diseases are comorbid with depression, because it can be extremely stressful to deal with an illness for years at a time,” says Naviaux. “If we can find ways to treat depression and suicidal ideation on a metabolic level, we may also help improve outcomes for the many diseases that lead to depression. Many chronic illnesses, such as post-traumatic stress disorder and chronic fatigue syndrome, are not lethal themselves unless they lead to suicidal thoughts and actions. If metabolomics can be used to identify the people at greatest risk, it could ultimately help us save more lives.”




No, a blood test cannot detect the specifics of anyone’s thoughts. Thank God!
. . . Thank God, indeed!